Developing a medication is a long process. It begins with the identification of therapeutic targets, to find the appropriate compounds to treat them. Once the drugs are identified, first, the scientific laboratory must carry out a preclinical investigation, to study the drug in vitro or in animal models; then clinical, with the study of the drug in the first human beings. The drug then enters phase 1, with trials in groups of healthy and volunteer patients. Phase 2 consists of tests with somewhat larger groups (100 to 500), to determine efficacy and appropriate dose. In phase 3, the sample is increased (up to 5000 patients) and side effects are monitored. Finally, in phase 4, the medicine is ready to be marketed.
Laboratories around the world are investigating drugs against COVID-19, which are at different stages of development. Now, a study published in The Lancet (a prestigious scientific journal, indicative of study quality) has published the first results of phase 3 of ‘a triple therapy’ (based on three drugs).
Promising results
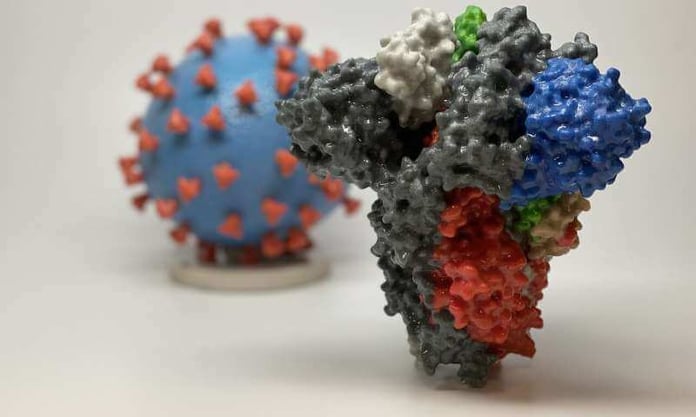
Therapy consisted of two weeks of interferon beta-1b plus lopinavir-ritonavir and ribavirin, which was started within 7 days after the onset of COVID-19 symptoms.
The conclusion is that triple therapy proved to be safe and more effective in reducing the duration of viral elimination (coronavirus was eliminated from the body more quickly) than in therapies with lopinavir-ritonavir (another drug that is in a clinical trial); but with a nuance: only in patients with mild to moderate disease, according to the first phase 3 trial, which involved 127 adults from six Hong Kong public hospitals.
No evidence in seriously ill patients
These early findings, as we have mentioned, do not include severe cases of COVID-19, and the authors emphasize the need for larger trials to examine the effectiveness of this triple combination in critically ill patients.
Viral load at its peak
Experience with influenza, which has a high viral load (the amount of virus that is present in an infected person’s body) at the time symptoms appear, suggests treating hospitalized patients with a combination of multiple medications Antivirals may be more effective than single-drug treatments, thus minimizing the risk of antiviral resistance. The authors hypothesized that this could be a possible therapeutic approach for COVID-19, in which the viral load also peaks at the time of symptom onset.
But again, more study is needed to see if it is effective in patients with more serious illnesses (in whom the virus has had more time to replicate).
Old known drugs
The drugs used in this triple therapy had already been used for the treatment of other diseases. Lopinavir-ritonavir is normally used to treat HIV; Ribavirin is a drug against the hepatitis C virus. The combination of both has already significantly reduced respiratory failure and death in hospitalized patients with the severe acute respiratory syndrome (caused by the SARS-CoV-1 coronavirus) during the 2003 outbreak.
Finally, interferon beta-1b, developed to treat multiple sclerosis (MS), reduces viral load and improves lung problems in animal studies of MERS-CoV coronavirus infection of the Middle East respiratory syndrome (MERS).
Limitations
The authors highlight several limitations in the study, such as that it was an open study in which both researchers and patients were aware of the treatment participants were receiving and did not have a placebo group. They also point out that the results can be confused by the subgroup of 34 patients within the combination group who were admitted 7 days or more after the onset of symptoms, and were not offered interferon beta-1b, but were analyzed as part of the group of combination.
This study presents a step toward finding a much-needed therapy for SARS-CoV-2. However, as the authors acknowledge, it is necessary to examine the efficacy of interferon beta-1b alone or in combination with other medications in treating critically ill or critically ill patients with COVID-19, and in comparison with placebo patients.