Until a certain point, it was a priori believed that since SARS-CoV-2 is a new virus, no one has immunity to it. However, several scientific works have already proven that the so-called innate immunity to coronavirus, based on cell memory, is not a fantasy. At the same time, scientists today believe that even more people may have an innate immunity to the “coronavirus” than previously thought.
Scientists recently analyzed six scientific studies that proved that the so-called specific T-cell immunity to COVID-19 is in 20-50% of people who have not previously met with it. The results of the work were published in the scientific journal BMJ.
The authors of two of the analyzed studies suggest that the reason for the emergence of immunity to the new “corona” is cross-immunity, which was formed after contact with other types of coronaviruses. As a result, contact with an infected SARS-CoV-2 in such people does not necessarily lead to infection, the infection does not necessarily lead to illness, and illness does not necessarily cause detectable antibodies. Scientists note that even in those regions where during the COVID-19 pandemic there was the largest increase in mortality, serological surveys after the peak showed that no more than one-fifth of the population have antibodies to SARS-CoV-2 : such 23% in New Zealand , 18% in New York, 11% in London and 12% in Madrid. For the general population, the numbers are much lower.
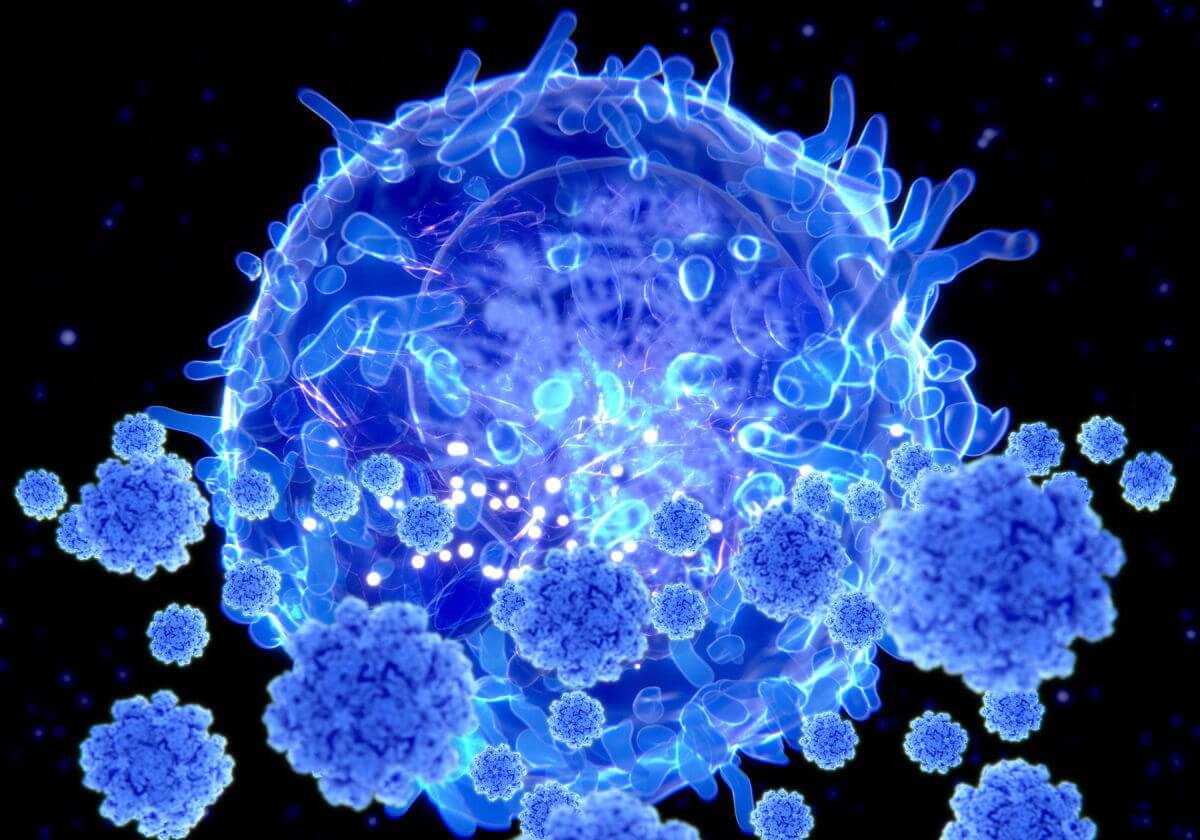
Therefore, today the importance of cellular immunity, which is formed as a result of contacts with viruses, comes to the fore. It is based on the so-called T-lymphocytes, which give the body’s cells a command to produce antibodies when they meet the virus again. As a result, even if antibodies are not detected in the blood of those who have been ill, this does not mean that they have no immunity: upon a new contact with the virus, T-lymphocytes start their “production”. As a result, people either do not show symptoms of the disease at all, or it goes away in an erased form. Today, virologists explain that 80% of those infected survive the new coronavirus infection easily, precisely by the work of T-cell immunity.
One of the studies conducted in the United States analyzed blood samples obtained from 2015 to 2018, – in 50% of them, T cells to SARS-CoV-2 were found. A similar study in the Netherlands identified 20% of blood samples with T cells. In Germany, reactive T cells were found in one-third of SARS-CoV-2 seronegative healthy donors (23 out of 68). In Singapore, a team of researchers analyzed blood samples taken from people who had no contact or personal history with SARS or COVID-19; 12 of 26 samples taken up to July 2019 showed T cells for SARS-CoV-2, as did 7 of 11 samples taken from humans who were seronegative for the virus. Similar studies with roughly the same data have been conducted in the UK and Sweden . Yes, all of these studies looked at small groups of people
And now they remembered that something similar happened during the swine flu pandemic in 2009. Many people tolerated it easily, which even then was explained by the presence of reactive T-cells formed as a result of meeting with genetically similar influenza viruses. A study conducted during the 2009 outbreak by the US Centers for Disease Control and Prevention (CDC) found that 33% of people over the age of 60 had cross-reactive antibodies to the H1N1 virus.
Today, scientists suggest that cross-immunity to SARS-CoV-2 can be developed not only in those who have once had seasonal human coronaviruses but even in those who have met the coronaviruses of some animals.
In theory, infectious disease outbreaks follow a specific trajectory. The number of new infections is rapidly increasing among the population without immunity. At some point in this growth, an inflection point should occur and the incidence will begin to fall. In the 1970s, a theory was born that defined this inflection point as the herd immunity threshold (HIT) and even the formula for determining it HIT = 1-1 / R0 (R0 is the average number of secondary cases). According to it, experts calculated that with SARS-CoV-2, in order to achieve herd immunity, at least 50% of people need to be ill. But there are other, more optimistic calculations – such should be from 10% to 20%. Scientists at Oxford University, for example, believe that when there are people with pre-existing immunity in the population, as studies of T lymphocytes can show,
Today, for example, everyone is studying the phenomenon of Sweden, where quarantine was abandoned at the beginning of the epidemic – and the number of cases and deaths was off the scale. Today, there in Stockholm, a city of 2 million people, only 50 people are hospitalized with COVID-19 . Has herd immunity really formed in Sweden? Swedish scientist Buggert conducted a study: studying close relatives of patients with confirmed COVID, he found T-cell responses in those who were seronegative or asymptomatic. While about 60% of family members produced antibodies, others had T-cell responses.
However, today, speaking of immunity, everyone is focusing on antibodies. And talk that antibodies to SARS-CoV-2 begin to weaken in just 2-3 months, fuel rumors of repeated infections. Even doctors are increasingly talking about them. “The increasing number of testimonies from colleagues about re-infections and, even worse, those occurring against the background of high antibody titers, is worrying,” said Moscow cardiologist Alexei Fedorov.
With T cells, things may be different: Singaporean scientists, for example, discovered reactive T cells to SARS-CoV-1 in patients who had recovered from the SARS coronavirus, 17 years (!) After infection. The metropolitan doctor, who wished to remain anonymous, who worked in intensive care in 2003, told the MK columnist that she herself had had SARS-CoV-1, which, it was believed, was not in Russia: “Almost all my colleagues had been ill – we had severe pneumonia, very similar to what we see now. However, this time, having contracted SARS-CoV-2, I suffered it almost without symptoms, on my legs, although I belong to the risk group. And colleagues who were sick then, now, continuing to work in intensive care units, either do not get infected or get sick easily. The SARS-CoV-1 and SARS-CoV-2 viruses are 80% genetically identical, and it is obvious that we have acquired cross-immunity. According to my estimates
“At the start of the pandemic, the key mantra was that we needed antibody data to understand who was infected and how many were protected,” wrote immunologists at Imperial College London. “As we learned more about this complex infection, it’s time to acknowledge that we also need data on T cells.”
So against the backdrop of a recent statement from a WHO representative that we are not even close to herd immunity, the results of studies on cellular immunity inspire some optimism.